Using Nitrous Oxide in the Office Outpatient Setting to Manage Pain and Anxiety
Dean Tortorelis, MD, FACS, Eric Freedman, MD, FACS, Ali Kasraeian, MD, FACS, Ramsey Nashed, MD, DABA, and Neil Baum, MD, FACS
Abstract: There is a trend among many physicians to move more procedures from the hospital and ambulatory surgical center into the office setting. The success of this transition requires that patients have a safe and comfortable experience without impacting the quality of outcomes. This article will discuss the adjunctive role of using nitrous oxide analgesia for in-office procedures generally, and the use of new technology in the form of the Nitrouseal® nitrous delivery system specifically, to manage the comfort of patients undergoing minimally invasive surgical procedures in an office setting. We will review our favorable experience with in-office use of the Nitrouseal® system with emphasis not only on patient outcomes, but further on the potential to enhance the efficiency and productivity of a physician’s practice.
Key words: Nitrous oxide, analgesia, outpatient procedures, practice efficiency, practice productivity, pain management, safety of inhaled nitrous oxide, contraindications to use of nitrous oxide, Nitrouseal®, MINISCAV®, minimal sedation.
Brief History of Medicinal Use of Nitrous Oxide In 1792, Joseph Priestly, the renowned English scientist and clergyman who discovered oxygen, also discovered nitrous oxide gas (N2O ). In 1799, Humphry Davy incidentally noted its analgesic action, but this fact was not recognized by surgeons. Nitrous oxide was used for public entertainment and during one of these demonstrations, Horace Wells, a dentist, realized the therapeutic applicability of the gas.
In the early 1860s the itinerant lecturer Gardner Quincy Colton and the dentist Thomas Evans were among the most fervent advocates of the use of N2O in dentistry.1
In 1895, dentists began administrating a mixture of nitrous oxide and oxygen through the patient’s nose for analgesic use during prolonged dental procedures. The dentists also noted that the patients regained full awareness very quickly after the procedure was completed, thus emphasizing the safety and rapid offset of the nitrous gas mixture. Nevertheless, it wasn’t until the 1970s that the dentistry profession adapted nitrous oxide on a wide scale for many common dental procedures because of its safety, and mild sedative and analgesic properties. The gas mixture commonly is administered by dentists using a nasal hood capable of being sterilized and reused. The fresh nitrous oxide/oxygen mixture is supplied to the nasal hood via tubing connected to a gas mixing device referred to as a “flowmeter.” The flowmeter is titratable, i.e. it has a control for varying the nitrous/oxygen concentration of the fresh gas up to a maximum of 70% so as to permit precise dosing to each patient. Typically, a separate tube associated with the nasal hood is connected to wall suction to scavenge the exhaled waste gas.
The Equipment A limitation exits with using “dental” nitrous delivery equipment in a physician’s office because scavenging through a nasal hood is ineffective containing and eliminating all exhaled nitrous. This limitation was overcome in 2010 with the introduction of the proprietary Nitrouseal® nitrous delivery system by SEDATION SYSTEMS LLC, St. Petersburg, FL 33715 (www.sedationsystems.com). Nitrouseal® features a patented, disposable, single-use, full-facemask2 and breathing circuit3 for providing fresh gas to the patient and for scavenging virtually the entire patient’s exhaled waste gas. Because of its relatively low cost, superior seal, fit, and waste gas elimination characteristics, Nitrouseal® met with immediate commercial success in the pediatric hospital environment where today it is typically used to minimally sedate patients during many procedures performed outside the operating room. In hospitals, wall suction is used to scavenge the patients‘ exhaled waste gas.
The final piece of the puzzle facilitating use of nitrous analgesia as an option for minimally invasive office procedures was the recent grant of FDA clearance to SEDATION SYSTEMS LLC for its MINISCAV® portable scavenger device. This suit-case sized, portable vacuum pump provides “wall suction” capability to medical offices. SEDATION SYSTEMS LLC is the only company in the U.S. that offers an FDA cleared scavenger, marketed under its MINISCAV® brand for use in the Nitrouseal® system, to evacuate exhaled waste gas from a medical office setting lacking “wall suction” capability. The complete Nitrouseal® nitrous delivery system for office use is illustrated in Figure 1, below.
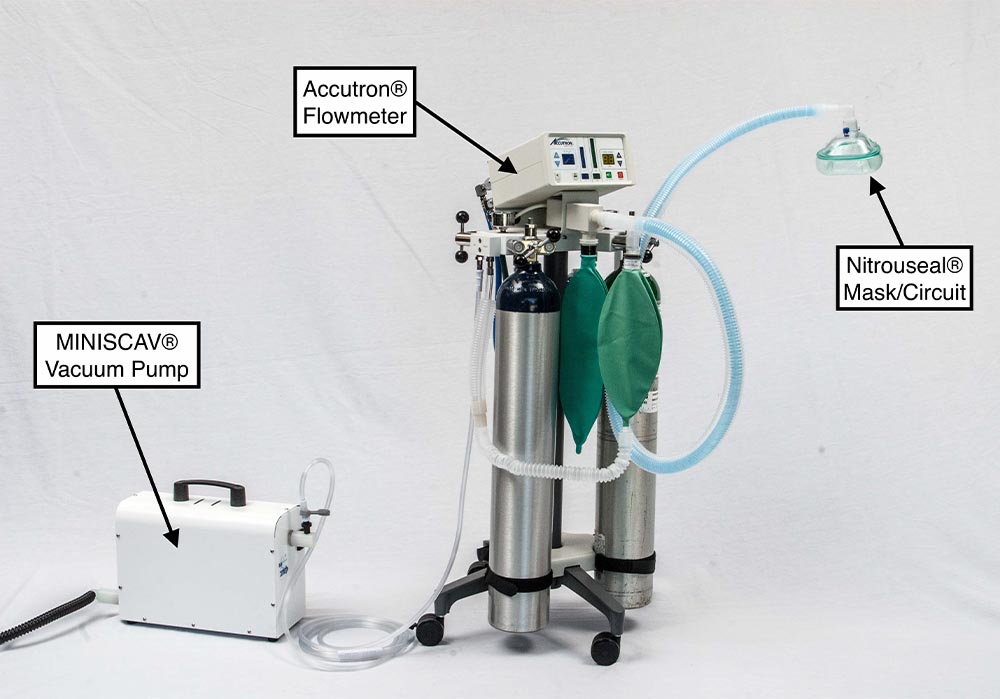
Figure 1: Nitrouseal® System
Safety and Physiology of Nitrous Oxide
Overall, nitrous oxide enjoys a large margin of safety. In many studies in pediatrics4 involving thousands of patients there were no incidences of major complications or apnea. The most frequently observed complications were nausea (1.6%), and vomiting (2.2%).
Nitrous oxide is not considered a respiratory depressant at clinical concentrations (30 – 70%). The decrease in respiratory rate seen is due to its anxiety reduction properties. Even at 70% nitrous patients can respond verbally to questions, so it is ideal for selfadministration during medical procedures. Because of its extremely low solubility in the blood, nitrous “wants” to come out of solution rapidly. The concentration in the brain rapidly equilibrates with the concentration in the alveoli. This explains the rapidity of onset of action while nitrous is being administered, and the rapidity of elimination once the inhaled nitrous is discontinued (i.e. usually less than a minute).
This rapid rate of offset enhances safety because any effect of nitrous will dissipate quickly because of the rapid elimination.
The low solubility of nitrous explains its affinity for any air pockets in the body, thus presenting a risk of expanding into any closed air pockets as in pneumothorax, bowel obstruction, or any air bubbles that may remain after inner ear or eye surgery. Patients with such conditions should avoid nitrous.
Also, this low solubility can lead to the theoretical concern for diffusion hypoxia. The scenario is one where after the nitrous inhalation is discontinued, it is rapidly eliminated from the blood stream into the alveoli. This, theoretically, can result in a displacement of oxygen in the alveoli resulting in a hypoxic concentration of gases therein. This concern is easily dealt with by simply having the patient breath/inhale 100% oxygen for a few minutes at the end of each nitrous administration.
The effects of nitrous on the cardiovascular system are minimal in vivo. The mild negative effect on myocardial contractility (this effect can be more pronounced in those with pre-existing left ventricular dysfunction) is countered by mild increase in sympathetic tone. In general there is hemodynamic stability
during nitrous oxide administration. Chronic or prolonged exposure to nitrous waste gas in a closed environment (e.g. work area) can lead to impairment of
Vitamin B12 metabolism. This can lead to megaloblastic anemia in healthy patients after 12 hrs. of continuous exposure to 50% nitrous. Patients with pre-existing Vitamin B12 deficiency would benefit from B-12 supplementation in conjunction with nitrous administration.
It has been documented that chronic exposure to nitrous oxide among female dental assistants who worked in offices where scavenging equipment was not used was associated with an increased risk of spontaneous abortion and reduced fertility.5
NIOSH (National Institute for Occupational Safety and Health) recommends that exposure to N2O be limited to 25 ppm on a time-weighted average (this is the
concentration of exposure multiplied by duration of exposure divided by an 8-hour work day).6
Therefore, it is imperative that doctors and office staff limit their exposure to nitrous oxide. The only way to do this is by using a scavenger system that draws a minimum of 45 L/minute of gas and vents to the outside of the building. In the absence of a central “wall suction” system, the only available portable FDA cleared scavenger system currently available meeting such performance criteria and suitable for use in a medical office is the aforementioned portable MINISCAV® vacuum pump offered by SEDATION SYSTEMS LLC.
Indications for Use of Nitrous Oxide
Nitrous oxide has a long history in dentistry as an effective inhaled analgesic for dental surgery. Additionally, inhaled nitrous oxide analgesia has found a number of indications in various medical practices such as, for example, colonoscopy/sigmoidoscopy, laser procedures, obstetrical labor pain, ophthalmic procedures, and joint injections.
In urology, nitrous oxide has been successfully used in a medical office for vasectomy, bladder biopsies, prostate biopsies, stent removal, and minimally invasive prostate procedures such as UroLift® and laser vaporization of the prostate.
Less commonly, self-administered nitrous oxide is reported for chronic pain from terminal illness and pain associated with cancer treatment.
Because of the excellent safety profile of nitrous oxide, it has been successfully used in children undergoing basic procedures including urinary catheterization, I/V injection starts, fracture reductions, Botox injections, lumbar puncture, venipuncture, or dressing changes. In these cases, nitrous has demonstrated a significant reduction in pain levels, allowing for a shorter recovery, and procedural efficiency.
For the anxious patient who is about to have a urologic procedure, nitrous oxide minimal sedation is a “game changer.” Due to the drug’s anxiolytic properties, the patient will be more relaxed. Because nitrous oxide has mild analgesic properties, it has the ability to raise patients’ pain threshold, and they will be more tolerant to how they perceive pain. The patient, by holding the mask on his/her face is psychologically distracted, moves less under stimulation, and thereby makes the physician’s job easier leading to enhanced outcomes.
Contraindications for Use of Nitrous Oxide Overall, nitrous oxide is a very safe drug with few absolute contraindications. Patients who have severe COPD, recent upper respiratory tract infections, or other pulmonary significant problems should not be considered candidates for the use of N2O.
Nitrous oxide dissipates from the blood stream very quickly and is able to enter airfilled cavities very rapidly. Thus N2O is contraindicated in patients where expansion of these air-filled cavities could compromise patient safety. This includes patients with pneumothorax, pulmonary blebs, air embolism, and bowel obstruction. We also recommend that N2O be avoided in any patient within two weeks of inner ear or eye surgery, i.e., cataract surgery with the implantation of an intraocular lens.
N2O interferes with the vitamin B-12 metabolism and can impair the production of the nucleotide thymine. Thus it can cause anemia in chronic exposure and in patients with a history of B-12 deficiency.
We recommend exercising caution using nitrous oxide in patients suffering from significant psychological disturbances, and current or recovering drug addicts.
Finally, N2O should be avoided in any patient who has Bleomycin therapy in the previous year. These patients are particularly sensitive to increase oxygen concentrations greater than 25% as this can result in the complication of pulmonary fibrosis.
Reported Results of Practice Cases
Since installing the Nitrouseal® system in our office practices, a total of two hundred seventy one (271) patients received nitrous sedation via self-administered, full-facemask inhalation as an adjunct to the following wide variety of urological procedures: vasectomies, cystoscopies, UroLift® implants, bladder biopsies, prostate biopsies and Botox injections.
In one practice, a physician, a co-author of this paper, reports:
“We began using Nitrous Oxide via mask inhalation (i.e. Nitrouseal®) as part of our clinic based Fusion Prostate biopsy program in late November 2017. We have expanded our experience, which now exceeds 30 patients, to include standard prostate biopsies. To date we have had no complications to report.”
The physician states further:
“… our patients who received Nitrous Oxide reported less pain and less anxiety. We also noticed that the patients seemed more relaxed and with less movement during both the calibration phase of the fusion biopsy and the actual biopsy portions of the procedure. In our active surveillance cohort, we have noticed patients reporting that their biopsy with Nitrous Oxide was subjectively “better” than previous biopsies without. Specifically, they reported less pain and less anxiety about the biopsy.”
Finally, this physician concludes:
“Since beginning our Nitrous Oxide program in our clinic, we have been wonderfully impressed with the results. Our patients have tolerated its safe administration with ease, without complication and, importantly, with great results.”
In another practice, a 2nd physician, also a co-author of this paper, reports:
“I started using Nitrous in my single Physician practice on June 21, 2017. I have done approx.. 110 Nitrous cases so far. 85 have been UroLifts. 8 have been difficult or anxious Vasectomies (most of my patients have just local), 16 have been cystos (anxiety, or PTSD with prior procedures, and the rare guy on Bladder Ca surveillance who wants Nitrous every time), and one prostate Bx.
The biggest improvement in safety & office flow is noticeable with the UroLift pts. Before they all had po sedation, and most were elderly, so mobilization was slow, all were wheel chair transport to their cars, & I was always concerned with the potential disaster of a post op fall or worse. And the degree of relaxation & pt. comfort is much better with Nitrous. None of my UroLift pts. get any premeds (sedation or analgesics) now.
The Nitrous has allowed me to do the difficult vasectomy cases that I would have otherwise sent to the Hospital.
And it has allowed the very anxious patients to accept doing cystos etc in the office environment.
This is much more time efficient than cases in the OR. I’ve done 12 UroLifts in a day in the office – could never have done that in the OR.
As for complications: No aborted cases. Only One case of nausea out of the lot (and we were suspicious he may have taken some sedatives before).
It has revolutionized the way I practice, and my confidence with doing procedures in the office. And my MA’s are all involved, and love it as well!”
Finally, a 3rd physician, yet still another coauthor of this paper, reports:
“Nitrous has changed my practice. It’s a no-brainer. It has allowed me to be more efficient and do cases in my office that I otherwise would have to do in the OR with the associated decrease in time efficiency. I can provide better care and service to my patients who are anxious about their upcoming office procedures. I have used Nitrouseal® for Vasectomies, TRUS biopsies, Saturation Biopsies, cystoscopies, Bladder Tumor fulgration, Stent removals, UroLift® procedures and Rezum®. We also plan on using it for UroNavFushion Biopsies.”
This physician adds:
“I started using Nitrous in January 2017 – since then I’ve used in my office close to 125 times. It’s a much safer alternative to P.O. anxiolytics – and patients are relieved that they can drive themselves to the office, have their procedure and drive home themselves … thus not having to arrange for a driver/spouse/friend to take time off. Elderly patients are also relieved with the safety and efficacy – and also not having to have pre-op testing for a hospital/Surgery. My staff also appreciates the use of nitrous and hears patients’ testimonials of how beneficial it was in decreasing the discomfort of procedures. Nitrous use has also distinguished my practice in the community. To date my group is adding Nitrous to 3 additional offices.”
The 3rd physician concludes by stating:
“We as urologists do thousands of procedures and don’t think much about the discomfort of our patients. When I started offering nitrous I was shocked at how many patients wanted it.”
Speaking collectively, our practices have not experienced any significant complications or adverse events using the Nitrouseal® system to administer nitrous oxide in our office settings. Nausea and dizziness were the most common side effects, but these resolved quickly within minutes after the N2O was discontinued. Vomiting has been reported in the literature as a side effect of N2O; however, we have not experienced this adverse effect in our practices. According to the literature the risk of vomiting is increased if concomitant opioids are administered or patient is NPO <2 hrs.7
Economic Benefits
There are many economic benefits using the Nitrouseal® analgesia system in a medical office practice setting. These include the following:
- Direct cash revenue for each nitrous administration: medical offices charge $100-200, many charge $125. Inasmuch as this fee is not covered by insurance, the office can offer it to their patients as a cash option. Most offices report very little resistance from patients at this price level.
- Site-differential reimbursement: most insurance companies (including MC) will compensate the professional fee at a higher amount if the same procedure CPT is done in an office vs. hospital or ASC. The insurance company can save the facility fee so they incentivize the physician to do more in the office. This along with the introduction of new minimally invasive procedures that can replace older more invasive procedures has encouraged the movement of many procedures to be performed in medical offices.
- Increased productivity for the physician: he/she can spend less time in a hospital surgeon’s lounge waiting for room turnover, and do more in the office. He/she can see patients, do paperwork or dictate reports, while the nurses are preparing the next patient. Every office that has started a Nitrouseal® nitrous delivery program has noticed a dramatic increase in productivity.
- Marketing advantages against competing medical practices: the word of mouth alone from satisfied and happy patients is invaluable and drives more patients to the practice. By combining that with a wellcrafted marketing campaign, a physician can achieve added growth in his/her practice.
- Increased staff satisfaction: staff personnel enjoy working in a thriving and successful practice and experiencing enhanced patient outcomes. This can increase retention of quality personnel and thus reduce staff turnover which is wasteful of productivity and increases costs.
Discussion
American healthcare is undergoing a significant change. We are moving from volume of care provided to the value of care we offer our patients.8 We are seeing a reduction in reimbursements for the services we provide, and increases in overhead expenses. As a result, our incomes are going to decrease. Therefore, it is imperative that we become more efficient in order to maintain our profitability.
Numerous studies have demonstrated that doctors are much more efficient practicing in their offices than in the hospital operating room or ambulatory treatment center. The use of technologically innovative systems such as Nitrouseal® to deliver nitrous analgesia gives the practitioner the ability to perform procedures in the office setting, in a safe environment, with enhanced patient satisfaction, and with resulting increased net practice revenue.
Conducting procedures in the formal operating room environment is a typically straight forward experience for the physician; however, sacrifices must also be made. First, being away from the office to conduct surgical cases seriously impairs physician efficiency. Even when a day of OR cases begins and flows as scheduled, turnover time in the hospital or ASC can cause gaps of 30-60 minutes between cases, time often spent drinking coffee in the doctor’s lounge without any access to the office EMR (in which case messages and patient results that inevitably accumulate must be dealt with at a later time, further compounding time lost). This inefficiency negatively affects almost all surgeons creating loss of productivity, reduced revenue, increased stress, and thus lower quality of life and satisfaction.
On the contrary, when working in the office the physician enjoys greater control of the schedule. An efficient practice can run several rooms at one time with a procedure being conducted in one room, a patient recovering in a second room, and a patient being prepared for a procedure or surgery in a third room. As a result, in-office procedures offer the physician clear economic advantages and significant improvement in productivity.
Patients also appreciate the benefits of inoffice procedures. The average patient is more comfortable in the office and with the office staff, than in a hospital or ASC and perceives large “facilities” such as hospitals as threatening (e.g., believing these are where “big and risky surgeries” are performed, and “hospitals are where people die”). Thus, patients are generally more reticent to accept procedures at hospitals or ASCs if an in-office option exists for them. Also scheduling barriers for in-office procedures are fewer than for hospital and ASC facilities.
There is also measurable stress and anxiety related to preparation for ASC facility or hospital procedures. Typically, for procedures performed in the office there is no fasting required, and no venipuncture for labs or IV placement. Additionally, offices don’t typically require separate anesthesia consent or advance directives. An established in-office patient doesn’t have to repeat a health history or insurance policy details prior to the procedure. Patients and family appreciate having less paper work to complete. Also, from a financial standpoint, patient co-pays and out of pocket costs are lower for office procedures. And since many office procedures are minimally invasive this allows patients with significant comorbidities to get the needed medical care with much lower risk.
Just as the doctor’s time is more efficiently spent in-office, patients who might spend most of a day at a facility even for a short OR case, are taken care of more quickly with office procedures. Importantly, safety concerns for elderly patients who could experience falls and even fractures after receiving anesthesia are much less likely when a procedure is performed in-office under minimal sedation with nitrous. This is uniformly appreciated by physicians, office staff, the patients, and their caregivers. Finally, as opposed to surgical facility requirements, many patients have the freedom to drive themselves home without an escort after an office procedure using nitrous oxide since it is so rapidly eliminated by the body. This is not the case with oral analgesics, or anxiolytic agents, where someone must accompany the patient to and from the office and the patient cannot resume daily activities for at least 4-6 hours.
The safety profile of nitrous along with its lack of respiratory depression, and its rapid elimination all contribute to its applicability of implementation in the medical office setting and its widespread use as a low-cost effective analgesic and anxiolytic providing more patient satisfaction with many urologic procedures.
We also want to mention that the use of nitrous oxide can be a practice builder. An anxious patient who has been made comfortable in the office will be a loyal patient for a very long time. Not only have you done a justice to that patient, but you have also enhanced your practice. Many of these patients who received nitrous oxide will refer your practice to their friends and family, some of whom will be anxious and want to be treated in an office that administers nitrous oxide sedation.
Most insurance companies will not cover the additional cost of nitrous oxide sedation, which means that this will be an out-ofpocket expense for the patient. We have found that a patient who desires being minimally sedated and an appointment that is less stressful will readily consider the charge a worthwhile expense.
The average cost to the patient for nitrous oxide is $50-125. Some offices build the cost of nitrous oxide sedation into their procedural fee structure. For example, offices that administer nitrous oxide just once a week will increase their revenue by $250 to $300 per month. Nitrous used once per day will increase revenue by approximately $1,400 per month based on a five-day workweek. This is an additional income of $17,000 per year. Nitrous oxide administered twice daily will increase office revenue by $34,500 per year. As the referred patients visit the office, the use of nitrous oxide sedation will increase over time.
Bottom Line:
Many diagnostic and therapeutic urological procedures can be performed easily and safely in the office with no sedation administration other than nitrous oxide, which is considered minimal sedation (Level I). In-office procedures offer many benefits to patients and physicians alike.
Nitrous is a low cost effective analgesic and anxiolytic. The safety profile of nitrous along with its lack of respiratory depression, and its rapid elimination all contribute to its beneficial application in many urologic procedures in the medical office setting.
We believe that with proper patient selection, nitrous oxide administered via the Nitrouseal® system can be an economic and productivity-enhancing asset to a urologic practice, to say nothing of improving patient outcomes and experience.
Conclusions:
Minimal nitrous sedation is an ideal lowcost analgesia for reducing pain and anxiety during many medical procedures. Moreover, it is beyond safe, proven by widespread and long use in dentistry and pediatric hospitals.
Until recently, it was not feasible to use nitrous sedation in a “medical” office setting because low-cost technology did not exist to solve the problem of preventing exhaled waste gas exposure to personnel.
With the advent of the Nitrouseal® fullface-mask and breathing circuit and FDA clearance of the MINISCAV® portable nitrous waste gas scavenger system, this problem has been solved.
Through use of “new” game-changing technology (i.e. the Nitrouseal® 3-component system*), it is now possible to move many invasive procedures previously performed only in a hospital or ASC to an office setting yielding synergistic benefits in productivity, net revenue, and Doctor and patient satisfaction. This conflates the trend of Insurance Companies to encourage increased office-based surgeries.
Nowhere is this more evident than in the field of Urology.
*Titratable Flowmeter (from Dentistry), proprietary full-face mask and breathing circuit to provide continuous flow of fresh gas and to capture all exhaled waste gas, and FDA-cleared portable vacuum pump.
Authors:
- Dr. Dean Tortorelis is Executive Director, Urology Associates Men’s Health Clinic, and Partner at Urology Associates Ltd, a division of Minnesota Urology, in Minneapolis, MN.
- Dr. Eric Freedman is President of Advanced Urology CA, in Sonora, California.
- Dr. Ali Kasraeian is Partner at Kasraeian Urology in Jacksonville, FL.
- Dr. Ramsey Nashed is a Board-Certified anesthesiologist, Medical Director of an orthopedic surgery center, and Co-Founder of SEDATION SYSTEMS LLC in St Petersburg, FL.
- Dr. Neil Baum is Professor of Clinical Urology at Tulane Medical School in New Orleans, LA.
References:
- Goerig M, Schulte, Am Esch J., History of Nitrous Oxide, Clinical Anesthesiology 15,313-338, 2001.
- U.S. Patent No. 8,336,549 granted December 25, 2012 entitled: Disposable Anesthesia Face Mask.
- U.S. Patent No. 8,826,905 granted September 9, 20114 entitled: Respiratory Face Mask and Breathing Circuit.
- Zier et al, Pediatric Emergency Care, Volume 27, Number 12, December 2011.
- Rowland AS, Baird DD, Weinberg CR, Shore DL, Shy CM, Wilcox AJ. Reduced Fertility Among Women Employed as Dental Assistants Exposed to High Levels of Nitrous Oxide, N Engl J Med. 1992;327(14):993-997.
- United States Department of Labor Occupational Safety and Health Administration website. https://www.osha.gov/dts/osta/anestheticgases/#C1. Published July 20, 1999. updated May 18, 2000, accessed July 9, 2017.
- Tsze DS, Mallory MD, Cravero JP. Practice Patterns and Adverse Events of Nitrous Oxide Sedation and Analgesia: A Report from the Pediatric Sedation Research Consortium. J. Pediatr., 2016 Feb. 169:260-5.e2.
- Katz C, Baum NH. Moving from Volume to Value, J. Med. Prac. Management, May\June 2018.
View the original White Papers document:



